
- Approval of ide-cel for adults who have relapsed after four or more prior lines of therapy follows clinical trials led by Dana-Farber Cancer Institute investigators
The Food and Drug Administration (FDA) has granted its first approval of a CAR T-cell therapy for adults with multiple myeloma, bringing welcome hope for patients eligible for the treatment, according to researchers and physicians at Dana-Farber Cancer Institute.
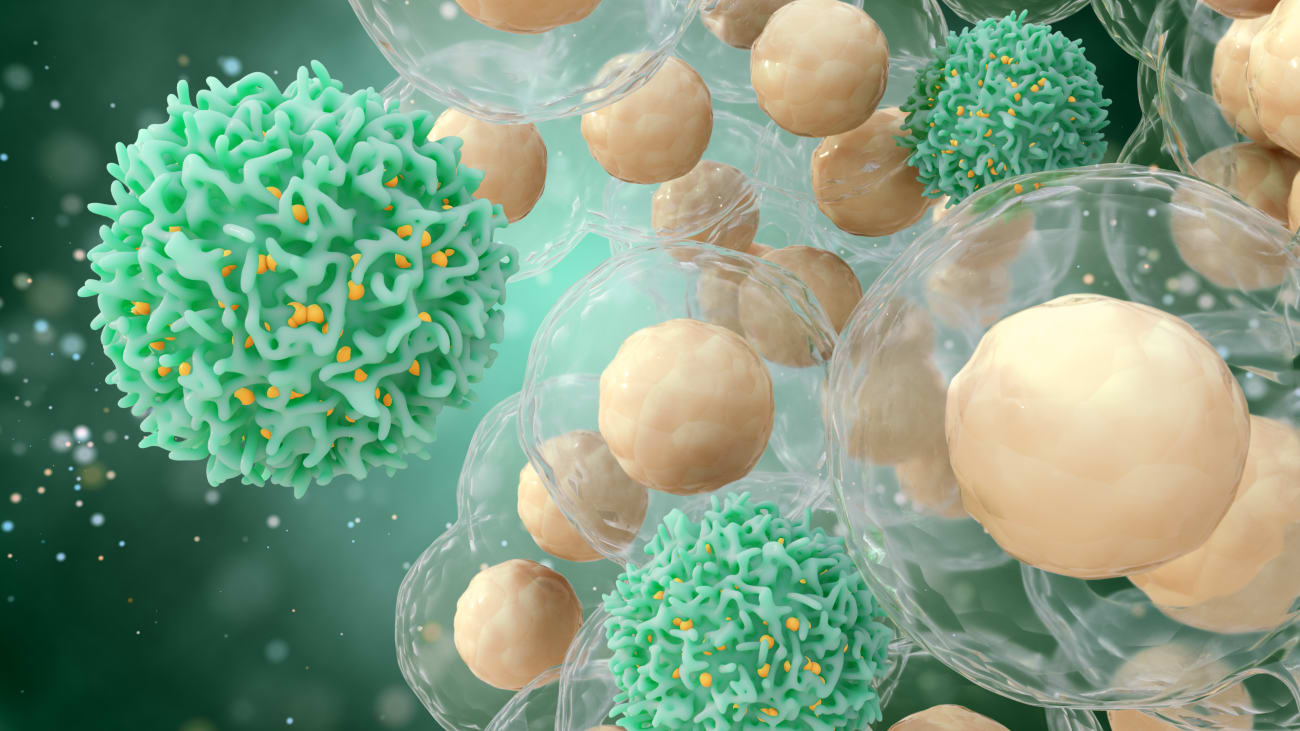
Approval of idecabtagene vicleucel (ide-cel) for adult patients with relapsed or refractory multiple myeloma after four or more prior lines of therapy comes after clinical trials showed the therapy can be highly effective in this group of patients, who previously have had few other treatment options. The therapy is made by genetically modifying patients’ own immune system T cells to target BCMA, a protein that is nearly universally expressed on multiple myeloma cells, leading to the death of those cells. Dana-Farber/Brigham and Women’s Cancer Center (DF/BWCC) will be a certified treatment center for the therapy.
 Nikhil Munshi, MD
Nikhil Munshi, MD
“As a treating physician, I often work with patients with relapsed and refractory multiple myeloma who are in critical need of new therapies. Now, with the approval of ide-cel as the first anti-BCMA CAR T-cell therapy, we are excited to finally be able to offer patients a new, effective personalized treatment option that is delivered through a single infusion,” said Nikhil Munshi, MD, Director of Basic and Correlative Science at Dana-Farber’s Jerome Lipper Multiple Myeloma Center, who led the phase 2 KarMMa clinical trial that tested the therapy in patients. “In the trial, ide-cel elicited rapid responses in the majority of patients, and these deep and durable responses were observed in patients who had already undergone treatment with three classes of therapies, including an immunomodulatory agent, a proteasome inhibitor, and an anti-CD38 antibody.”
Multiple myeloma is a cancer of plasma cells, which are white blood cells responsible for making antibodies against invasive germs. The disease is diagnosed in about 35,000 people in the United States each year, making it the second-most common blood cancer in adults. Among African Americans, it is the most common blood cancer.
The KarMMa trial involved 127 patients who had active myeloma after receiving at least three previous therapies. At a median follow-up of 13.3 months, 72% of the efficacy evaluable patients (n=100) had a response – a measurable reduction in their cancer – and 28% had a complete response or better. Median duration of response was 11 months for patients who achieved a partial response and 19 months for those who achieving a complete response. Of the 28 patients who achieved a complete response, an estimated 65% had a remission lasting at least 12 months.
These outcomes were superior to those achieved by standard treatments for multiple-relapsed myeloma. Other treatments have a response rate of 20-30% and a progression-free survival of 2-4 months.
The most common side effects of treatment were low blood-cell counts and cytokine release syndrome, a frequent follow-on of CAR T-cell therapy in which the immune system generates an intensive inflammatory response. Clinicians have developed effective treatments for this condition.
DF/BWCC offers all FDA-approved CAR T-cell therapies in blood cancers, including axicabtagene ciloleucel (Yescarta); tisagenlecleucel (Kymriah), and lisocabtagene maraleucel (Breyanzi) for aggressive, relapsed and/or refractory diffuse large B-cell lymphoma, primary mediastinal B-cell lymphoma, and transformed follicular lymphoma; axi-cel for relapsed or refractory follicular lymphoma; and brexucabtagene autoleucel (Tecartus) for relapsed/refractory mantle cell lymphoma. Clinical trials of CAR T-cell therapies for other types of blood cancers are underway at DF/BWCC and include trials of these therapies earlier in treatment and in combination with other immunotherapies.
For more information about CAR T-cell therapy, click here.
