
A melanoma therapeutic vaccine is a type of personalized cancer vaccine that is intended to train the immune system to fight cancer cells in a way that lasts many years. These novel vaccines are personally tailored to recognize the mutations present in an individual’s tumor cells. They are different from vaccines for infectious diseases, which are typically given to as many people as possible in a community to prevent a virus from spreading.
Currently, no personalized melanoma vaccines are approved medicines, though several have been tested in clinical trials. A personalized RNA vaccine has recently shown promising data in patients with high-risk melanoma.
Researchers at Dana-Farber in collaboration with experts at the Broad Institute recognized the possibility of personalizing cancer vaccines over a decade ago. Dana-Farber researchers translated the ability to identify unique, personalized flags on cancer cells into a vaccine that trains the immune system to recognize them. That vaccine, called NeoVax, was one of the first personalized cancer vaccines to be tested in patients.
“The ability to vaccinate against a tumor’s mutations is a big deal,” says Patrick Ott, MD, director of the Center for Cancer Vaccines at Dana-Farber. “In the past, we could not identify a tumor’s mutations timely enough to allow manufacture of a custom-made vaccine for a patient. Now, we can not only do it, but we can do it within a timeframe that is reasonable for patient care.”
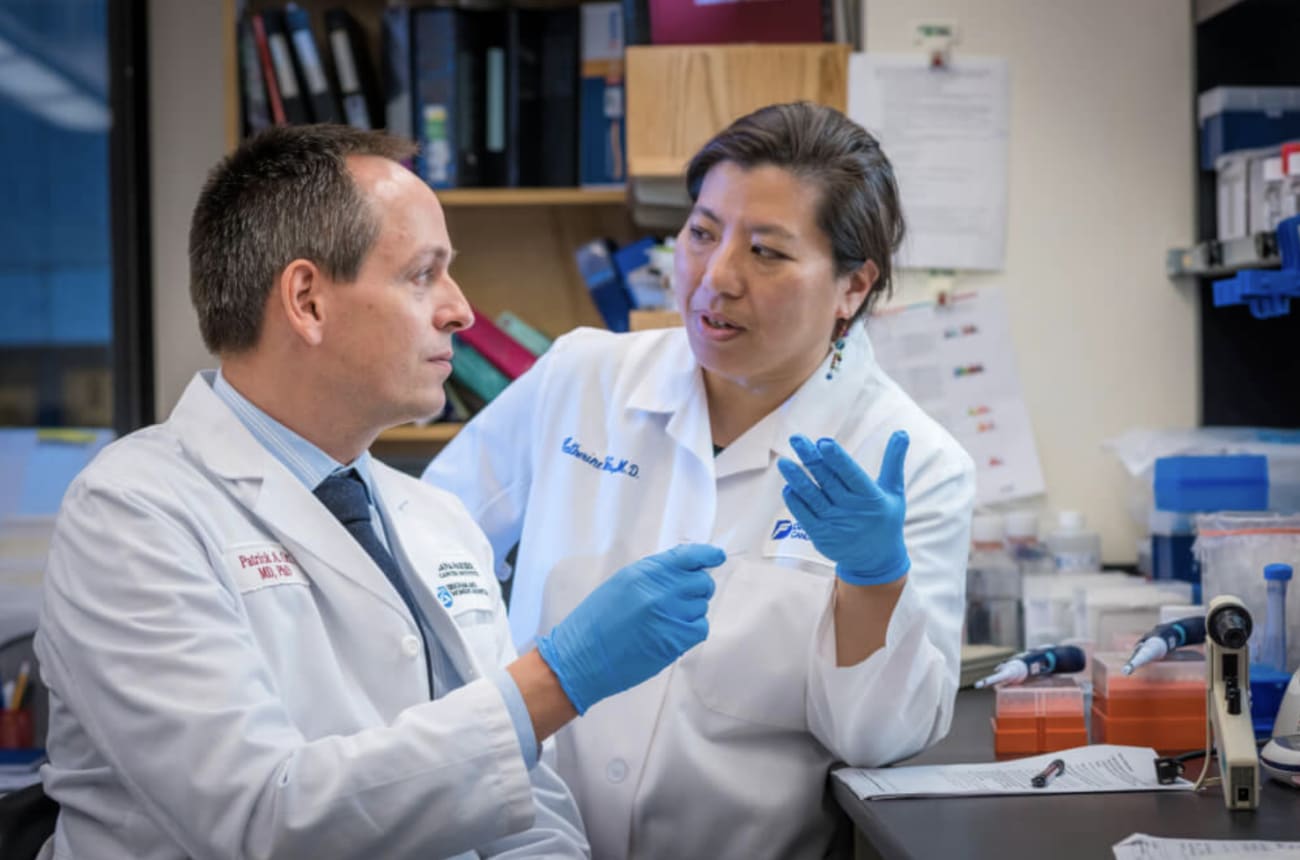
Ott and Catherine Wu, MD, chief of the Division of Stem Cell Transplantation and Cellular Therapies at Dana-Farber, along with their team, were the first to bring this novel concept for a personalized medicine to regulators at the U.S. Food and Drug Administration to find a way to evaluate it in patients safely. Their first clinical trials and subsequent trials of the medicine showed that the strategy had merit.
Who can get a melanoma vaccine?
Melanoma vaccines are used to treat people with melanoma. They are currently only available in clinical trials, which may have specific criteria for a patient to be eligible.
A phase 2 clinical trial of an mRNA-based personalized melanoma vaccine is currently open at Dana-Farber and across the nation for certain patients with high-risk metastatic melanoma.
Dana-Farber experts are testing the personalized NeoVax vaccine for melanoma in smaller trials that are exploring how best to combine the vaccine with other agents that stimulate the immune system.
Learn more about personalized cancer vaccine clinical trials at Dana-Farber.
Why are melanoma vaccines personalized?
When you get a vaccine for a virus, the vaccine is not personalized. You and the person behind you in the vaccination line will likely get the same formulation. That is because viruses are already recognized by the human immune system to be foreign invaders. Vaccines for viruses give the immune system a leg up by giving it advanced training to recognize these invaders.
Cancer cells, however, are not foreign invaders. They originate from our own healthy cells. A longtime quest in cancer immunology has been to find a way to make cancer medicines that distinguish cancer cells from those healthy cells. Many side effects from cancer medicines occur when the medicine harms both cancer cells and healthy cells.
Personalized vaccines are a way to identify flags that precisely distinguish an individual’s cancer cells from healthy cells and train the immune system to seek them out. Those flags are the result of the mutations that have occurred in an individual’s cancer. The exact mutations will vary from one individual to another.
“Mutations are the long elusive target for cancer vaccines,” says Ott. “Vaccinating against tumor mutations mimics vaccinating against a virus.”
Learn more about personalized cancer vaccines.
How are melanoma vaccines personalized?
The NeoVax vaccine involves targeting “neoantigens” on cancer cells. These are antigens — distinctive protein fragments — on the surface of cancer cells that are produced by mutations in the cancer cell’s DNA. Many neoantigens are specific to an individual patient’s cancer and aren’t found in normal cells.
NeoVax is made by sequencing the genetic information of a patient’s tumor to identify neoantigens produced by mutations in that tumor. The vaccine incorporates copies of as many as 20 neoantigens into the vaccine, which is given to the patient along with other medicines to activate the immune response. The neoantigens are intended to steer the immune response to the site of the tumor.
How is research improving melanoma vaccines?
Dana-Farber researchers are trying to find ways to improve the performance of melanoma vaccines. They did the seminal clinical research that showed that personalized vaccines work to stimulate immune cells to recognize and fight cancer.
The immune system and its interaction with cancer cells is complex. Cancer cells are stealthy and have many ways to evade and suppress the immune system. In addition, there are many types of immune cells with different skills and ways of working together.
Research at Dana-Farber aims to find ways to combine cancer vaccines with other immunotherapies to fine tune the immune system’s ability to fight an individual’s cancer. This research is being carried out in the laboratory and in clinical trials.
“It is wonderful that personalized cancer vaccines are advancing and showing responses in patients,” says Ott. “We believe we can improve that response, so our efforts are focused on learning how to do that step by step.”
What other personalized vaccines are in development?
At Dana-Farber, the NeoVax personalized vaccine is in clinical trials for patients with renal cell carcinoma (kidney cancer), glioblastoma multiforme (a form of brain cancer), ovarian cancer, and chronic leukemia and lymphoma.
